Diabetic retinopathy is a major diabetic eye problem and a leading cause of blindness among people with diabetes. It has deep links to kidney damage – diabetic nephropathy. People with diabetic nephropathy are at a higher risk of getting diabetic retinopathy. Diabetic retinopathy is a cause for concern as the number of cases have increased over the years. It has led to numerous cases of permanent vision loss and still the level of awareness is quite low.
What is Diabetic Retinopathy?
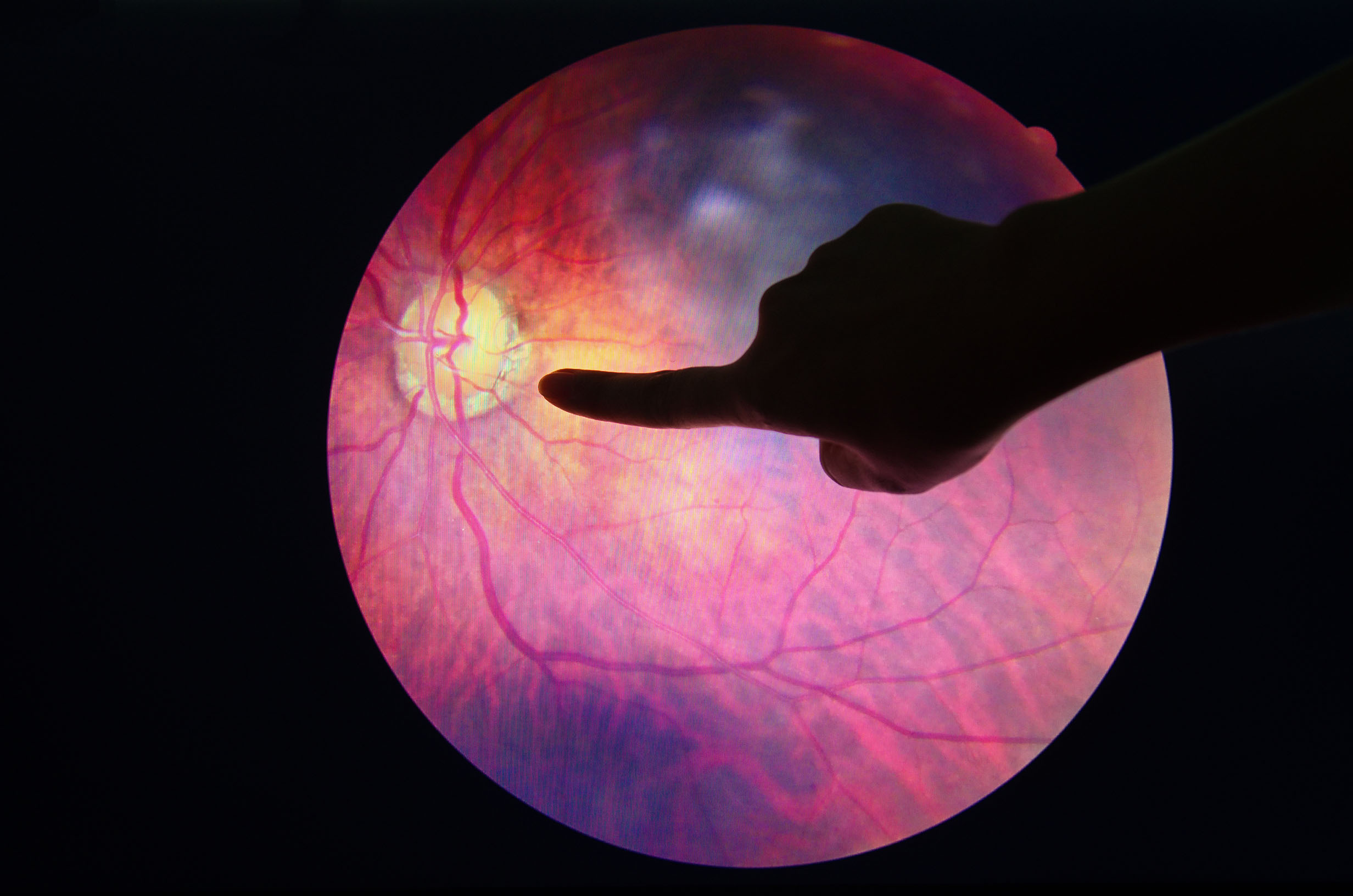
Diabetic retinopathy affects both blood vessels and nerves of the retina. All diabetic retinopathy stages are progressive damage to blood vessels and nerves. If left unmanaged, it leads to permanent vision loss.
Diabetic retinopathy is common in both type 1 and type 2 diabetes. This condition usually occurs in people who also have diabetic nephropathy. People who are medically managed for diabetic nephropathy have improvement in their diabetic retinopathy.
In the early stages, diabetic retinopathy does not manifest in the form of any symptoms. Diabetic retinopathy symptoms show up only in the later stages when considerable damage is done. It is for this reason, getting frequent eye examinations is vital. Among these tests, if there is presence of microaneurysms, it is a clinical sign that you have diabetic retinopathy.
Retina and Vision
The retina is like a cinema screen. A movie screen reflects light coming from the projector. Similarly, a retina receives light from objects and converts them into electrical impulses. The retina is a thin tissue layer and is light-sensitive. It is full of nerve fibers and many small blood vessels that function along with the retina to provide vision. Retina also consists of rods and cones. Rods assist in providing vision in the dark and dim light and cones assist vision in daylight. Without a properly functioning retina, there is vision loss.
How is Diabetic Retinopathy caused?
Blood Vessel Damage
In people with diabetes, chronic high blood sugar levels bring about early changes in their retinae. As early as five years in the age of diabetes, people develop certain conditions like narrowing of retinal arteries along with reduced blood flow to the retina.
Rise in blood sugar levels lead to slow death of small blood vessels. This is caused when sorbitol gets deposited in the cells as the body cannot convert it into fructose. This sorbitol causes increased production of free radicals, reduces cell permeability and production of AGEs (advanced glycation end products). AGEs are major contributors to cell damage. AGEs are responsible for diabetes complications.
Nerve Damage
Nerves of retina also undergo changes in all diabetic retinopathy stages. As a matter of fact, nerve damage starts very early (in weeks after the onset) in people with diabetes.
Retina is full of nerves and blood vessels. The function of these nerves and neurovascular units are to provide nutrients and oxygen and remove cellular waste. They assist in providing sympathetic nerve activities like constriction and dilation of blood vessels, flow of blood through blood vessels, maintaining internal eye pressure, and retinal irradiance and illumination.
All these functions are essential for normal vision. When considering diabetic retinopathy stages, nerve damage occurs even before there are any microaneurysms, lipid leakage, and retinal hemorrhages.
In the first of diabetic retinopathy stages, retinal blood vessels have reduced dilation and contraction. This is due to neurovascular changes in the retina. Even before the development of diabetic retinopathy, people might have reduced ability to see in the dark and an inability to sense subtle contrasts of colors. This is also due to neurovascular damage.
Nerve damage starts with insulin receptors in the retina. Incidentally, insulin receptors in the retina (unlike other organs’ receptors) also facilitate nerve growth, development and nerve survival. So, along with the onset of diabetes, nerve damage in retina immediately starts with insulin resistance.
Nerves start to die due to the presence of free radicals and accumulation of AGEs (advanced glycation end products)which have toxic effects on nerves of retina. AGEs react with the nerve cells and decay them. They also promote birth of new and unstable blood vessels that might cause diabetic macular edema. This process is called neovascularization.
In addition to high blood sugar levels, systemic inflammation and lipid metabolism also contribute to diabetic retinopathy with blood vessel and nerve damage.