Diabetes Complications and Eye Disease
Diabetes affects 3- 4 % of the world population. India is about to become the diabetes capital of the world with the second highest number of people with diabetes. Around 40 million people in India have diabetes and 50% of these show some signs of diabetic retinopathy at any given point.
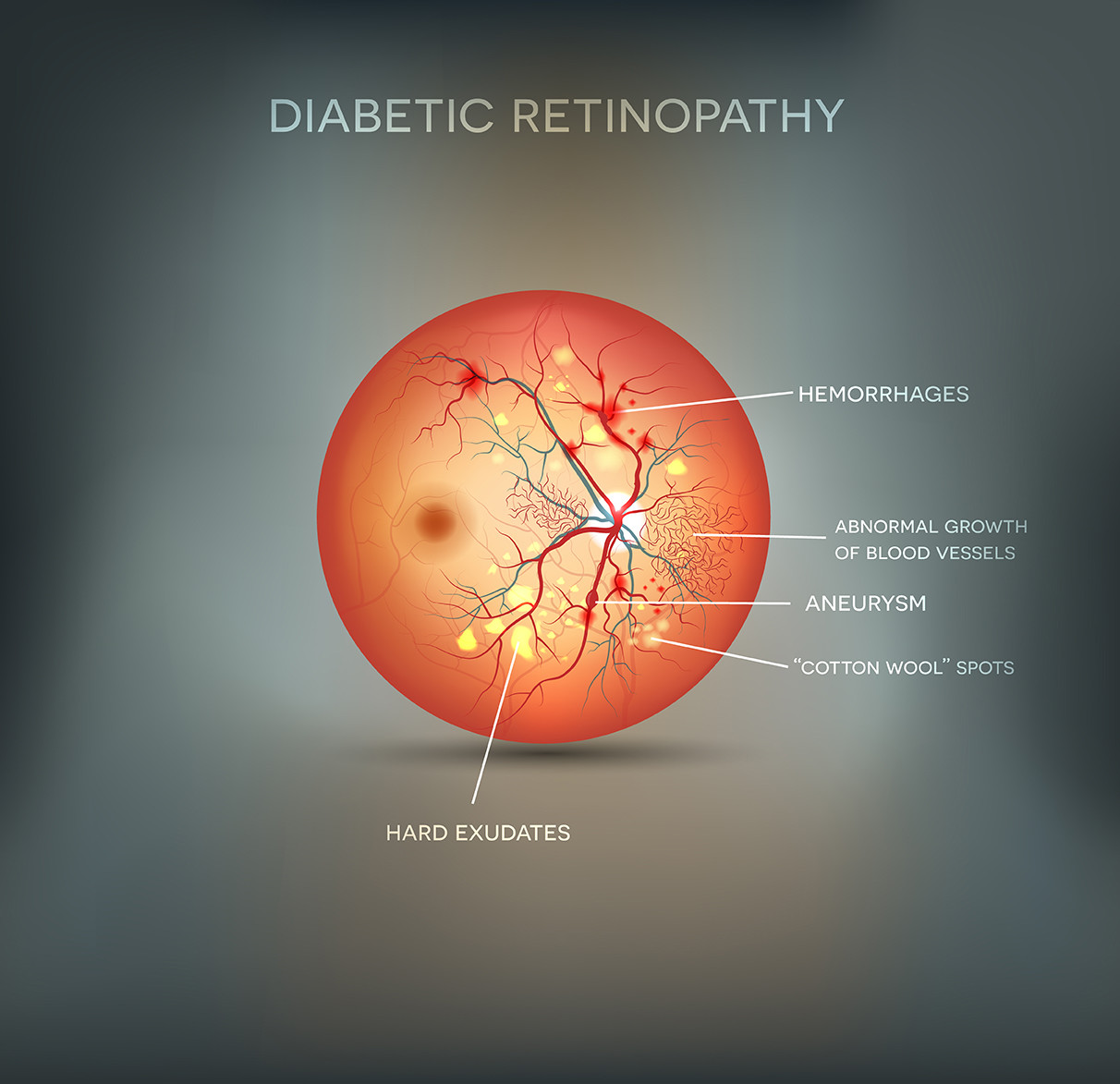
Diabetic retinopathy is a complication of diabetes and a leading cause of blindness. It occurs when diabetes damages the blood vessels of the retina. Retina is the light-sensitive nerve layer of that line the back of the eye and is necessary for good vision. Retina converts the light that enter the eye into nerve signals and are sent to the brain. Diabetic retinopathy occurs when high blood sugar damages or clogs the blood within the retina. Diabetic Retinopathy is responsible for 5% of the total blindness in the world.
Diabetic retinopathy affects both Type I and Type II diabetes. The risk of developing diabetic retinopathy increases with the duration of diabetes. After 15-20 years of diabetes:
- 80% of patients will develop some form of diabetic retinopathy
- 10% will develop severe visual loss
- 2% of patients will become blind.
- 20% of patients will have diabetic retinopathy at the time of detection of diabetes.
Signs and Symptoms
Diabetic Retinopathy initially has no symptoms. Symptoms only develop when the damage to the eye is severe. Hence, do not wait for symptoms to develop and go for regular eye checkups.
- Blurring of vision
- Dark spots moving in your vision called floaters
- Missing areas of vision
- Difficulty in seeing at night
The above symptoms may not necessarily mean that you have diabetic retinopathy, but you need to see an eye specialist if you experience any of these symptoms. Patient education is an important aspect in the detection and treatment of diabetic retinopathy.
Everybody with diabetes is at risk of developing diabetic retinopathy. Hence everybody with diabetes should have a detailed dilated eye examination at least once in a year. Diabetics are also at increased risk of developing cataract and glaucoma.
The following measures may help you in reducing the risk of developing diabetic retinopathy
- Studies have shown that long term good control of the diabetes reduces the risk of developing retinopathy.
- Checking your blood pressure and cholesterol regularly and keeping them under control would reduce the progression of retinopathy.
- Stop smoking.
- Regular eye check up
- Take your medications as prescribed by your doctor, regular exercise and a good diet will reduce the progression of the disease.
Diabetes and diabetic retinopathy are progressive conditions and hence regular follow up with your doctor is very important to detect and treat any changes. Goal of treatment is to prevent visual loss. Treatment depends on the stage of the disease. Early stages do not need treatment, but need to be regularly checked to detect any progression.
The main treatment options for diabetic retinopathy include:
LASER also called photocoagulation is done when leakage from the blood vessels affects the vision. Laser helps to prevent bleeding and decrease swelling in the retina. Laser cannot restore vision already lost due to retinal damage.
intravitreal injection or injection into the eyeball. Certain drugs are injected into the eyeball which prevents the damaged blood vessels from leaking. This reduces the swelling and can improve vision. Combination of lasers and injections are also effective
SURGERY: Vitrectomy is done if there is bleeding in the vitreous which is the gel in the center of the eye. Retinal microsurgery is done to remove scar tissue and retinal reattachment in advanced cases
If you have already lost vision due to diabetic retinopathy, low vision devices may be prescribed to make the most of your remaining vision.